On 20/04/2019, Fostair triggered a blackout when dosage was increased - see the second post on Facebook/@aspirin2relief. This confirms the suggestion that beclomethasone was causing the blackouts experienced when Qvar was used regularly (see below.)
"Asthma is a common condition caused by inflammation in the smaller airways of the lungs. The inflammation irritates the muscles around the airways and causes them to constrict. This causes your airways to narrow. It is then more difficult for air to get in and out of your lungs. This causes the typical symptoms of wheeze, chest tightness and shortness of breath. The inflammation also causes the lining of your airways to make extra mucus which causes coughing." patient.infoContents:
Asthma developed only in winter on coasts with cold currents.
Diary.
Blackouts happened after using a steroidal 'preventer' for asthma.
Aspirin can prevent wheezing at night and is helpful against asthma in some daily situations.
Conclusion
Asthma developed only in winter on coasts with cold currents.
As a child, I had just one asthma attack. It was on a bus in Cape Town¹, in the winter of 1970. My parents took me off the bus immediately and I recovered.
¹Cape Town has cold Atlantic water to the west and its Mediterranean climate means wet, windy winters (with hot, dry summers.) To the east of the city, nearby False Bay has warm water from the Indian Ocean, and it might account for some or most of the humidity in the city's air in winter (Summers are extremely dry in False Bay.) The sea temperature at Cape Town ranges between an average of 15°C in winter and 18°C in summer.Having just immigrated to South Africa from Bristol, we moved on immediately to the 'Highveld', - to near Johannesburg (elev. 5751 ft.) and I had no further indications of asthma for 23 years.² N.B. Highveld winters were cold but very dry.
I forgot about asthma for 23 years after leaving Cape Town and also had no problem for another 11 years in Iowa City, USA. The South African Highveld and Iowa are both far from a frigid sea and have dry air in winter. The air gets extremely dry on the Highveld, and you'd never survive the winter without camphor cream on the hands. In spite of winter snowfall in Iowa, the atmosphere becomes dry there too, thanks to Canadian air that moves south. (The summers there are notably humid.) Even cycling daily on snow at 6 a.m. didn't induce asthma. People there tend to buy humidifiers, something that is not easy to find in the shops in Plymouth.
²Some of my South African asthma-free time was spent in the eastern regions, closer to where the Indian Ocean's surface temperature ranges between 23°C and 27°C. As an adult, I did have a reaction to inhalation of old carpet dust in the Eastern Cape Province, but I never thought of the word "asthma" again until 2006 in Plymouth, on the English Channel with its cold currents.I moved to Plymouth in 2004 where sea temperature³ is on average a few degrees colder than at Cape Town. I noticed some wheezing at bed-time in 2005 and this puzzled me (having forgotten that I'd ever had asthma) but I suspected that it had something to do with house dust and air temperature. A couple of years went by and true asthma began to take place, e.g. I'd wonder why I was tight-chested after an evening shower and could still sense the tight chest after driving to a pub in town. The asthma was moderate and occasional for a few years but, in July 2014, its severity and frequency increased alarmingly. I began to have extreme difficulty breathing at night, and (when relying only on salbutamol reliever) wheezing became so loud that just the noise of it would prevent sleep altogether.
No asthma occurred on summer field trips in the Southern Ocean, including a week at the Antarctic ice shelf: The atmosphere on the Antarctic coast is dry because the water is so cold that moisture condenses out of the air above it.
³Sea temperature at Plymouth ranges between 10°C and 16°C averages, not very dissimilar from that in Cape Town.
Perhaps we could call asthma in south-west England "Gulf Stream asthma": The Gulf Stream current is the source of the moisture in the air here because its warm water moves toward us from the Gulf of Mexico. Once the moisture gets here it is cooled above our local waters but stays in the air. Cold weather and humidity in combination causes asthma for many. When we are lucky enough in winter to have the Jet Stream push much colder air down from the North during high atmospheric pressure, it is dry air and quickly relieves the land of humidity. Likewise, it relieves one of asthma totally.
Diary
A recent conclusion: ASTHMA ON THE COAST HAPPENS WHEN LOW TEMPERATURE AND HIGH HUMIDITY OCCUR TOGETHER:
06 January 2017:
The northerly wind on Wednesday brought a new level of coldness but soon it was also noticeable that the road surfaces were dry again. The dry air relieved me entirely from any need for asthma treatments.
22 January 2017:
Low atmospheric temperatures have arrived again after a warmer spell, but no asthma occurred because the air is dry (comes from snowy north of Europe.)
19 Feb 2017:
Day-time mists last week led me to discover that real-time humidity measurements are found simply by Googling "humidity plymouth". Persistent asthma was associated with readings near 100%. Using Serevent first thing made it possible to return to the workplace and stay there, even when humidity was at 100%. - The remedy was to use Serevent at 5:30 AM and not in the evening beforehand: It works well when used sparingly, ideally less than once in a 24 hour cycle.
Today, the air seemed better and the reading was 85%. After lunch, however, those mists were back and humidity was 98%. Walking in damp woodland with up-hill climbs would have been difficult. Sucking on a dispersible aspirin in the warm car can clear the breathing in such circumstances if the temperature is up near 11ºC, but a strenuous walk would have been impossible without a puff of Serevent first. (p.s. Serevent brings drowsiness and a susceptibility to migraine.)
98% is a typical RH reading in Plymouth when asthma is likely to occur.
7 Jan 2018 Amazingly, not a trace of wheeze or asthma after a shower this evening. Then I realized that a cold front from the North has done it again: brought drier air. Checked with a google search and humidity is dropping by the minute: had reached 66% when I saved this screenshot. (It's been above 82% all week and reached 92% twice, causing a need for Salamol and for Serevent when Salamol didn't help enough.)
66% RH: The Polar jet stream pushes dry air southward to Plymouth. The dry air means total relief from asthma, even in the coldest months.
8 Jan 2018 Relief was short-lived. Atmospheric humidity climbed again in the night and is back at 86% (precipitation is still at 0%.) Asthma built up through the early hours and is quite bad now at 4 AM. Plymouth is known for its asthma suifferers. It seems that the wide swings in atmospheric humidly here are a key factor.
|
Blackouts happened after using a steroidal 'preventer' for asthma. (Also see Part ii, below.)
A problem began after I was put onto beclomethasone dipropionate (Qvar®) in 2011. I started to have fainting episodes. Just before a blackout commenced, I would get a nightmarish sensation - like a grim sort of 'deja-vu' - and then lose consciousness. (Recalling those episodes, one wouldn't wish them on a worst enemy. There is struggle for inner balance while consciousness is lost. There is a sense that the outcome is unknown.)
At the time, I had been taking supplemental potassium for lowering of blood pressure. I stopped taking that but the collapses still happened. (A high blood pressure reading at the GP surgery had been a false alarm and I had used no other substance to control b.p.) It dawned on me that beclomethasone might be having a hormonal effect on my blood pressure because it is a synthetic hormone. Why suspect blood pressure?: In my twenties, I was turned away from blood donation because of a low blood pressure reading, which suggests that I might be affected by anything that further reduces my b.p.. (This is detailed in Part ii below.)
With the new severity of asthma and wheezing that began in July 2014, I tried alternative asthma drugs (see Part ii.) However, I was beginning to think I'd never manage without the reliability of steroidal beclomethasone.
On trying a schedule of beclomethasone again in 2016, i.e. the fourth attempt.
>> 5th June 2016. After a break of 18 months, I have started using beclomethasone dipropionate again, once per day to improve sleep. Aspirin was still working as described, but it was not preventing me from waking too early in the morning because of a slowly increasing asthma if the bed became cold. - It was becoming quite burdensome to have a hot honey drink with aspirin every time this happened. So far, one puff of beclomethasone in the afternoon has had good effect. I still recommend aspirin for being able to prevent bad wheezing in the night. I will still use it before showering and keep it handy as a 'supplement' to my single daily dose of beclomethasone. >> 6th June 2016. The eerie sensation that precedes blacking out (as described below) has returned after 3 days back on beclomethasone, but only briefly. >> 8 pm, 23 June 2016. I just had one of the blackouts that got this blog started a couple of years ago. I recognized it coming, turned off the stove-top and lay down quickly. It passed in a few minutes. I am now convinced that beclomethasone gives me blackouts, even though I had started using it less than once per day. >> 26 June 2016. I was waking from an afternoon nap when I went into a severe blacking out state (quite unnerving and feels life-threatening.) I managed to stay conscious by breathing faster and moving my body intuitively. I did not feel that I could get up for water until it passed. I am now 100% certain that Beclomethosone was the cause of the blackouts that began in 2011.
(August 2017) 'have wondered if the medium in which Qvar is transferred might be a factor in the blacking out because 'have sensed a similar, but much less frequent, vulnerability after using Serevent (obviously, a different chemical in a dry medium.)
A Google search can show that inhaled steroids are commonly regarded as being 'low risk' in terms of side-effects. However, Budesonide now comes with a flyer that declares rare side-effects as follows: "too much or too little cortisol in the blood" and "low blood pressure or collapse". That declaration supports what is discussed in Part ii, below. (Also see bit.ly/ICSdanger or bit.ly/pneuflut which showed that a combination of inhaled steroid (fluticasone) and salmeterol was raising levels of lethal pneumonia in 2013, with the steroid then being the cause.)
THERE IS NO SUGGESTION THAT ASPIRIN BE GIVEN TO CHILDREN.
In January 2015, I noticed that aspirin had relieved a tight chest one morning. Then, I noticed that I'd made a similar observation previously in this blog. I began to suck on 'dispersible' aspirins at key times in the day, and it kept the asthma down. It stopped all serious wheezing at night: There has never been a re-occurrence of the loud, sleep-depriving wheezing of July 2014 since I then began taking aspirin before bed. If I still get a stubborn asthma in a very 'triggery' situation (e.g. after having a shower in a cold bathroom, now remedied by pre-heating the bathroom), I can use salmeterol xinafoate, a reliever in powder form. (Even when I was using steroidal beclomethasone, I needed the additional help of a reliever sometimes.) This 'stubborn asthma' occurred once or twice per week in December 2015.Prevention of night-time, loud wheezing has remained a very reliable effect of taking aspirin since January 2015. (Some wheezing can still occur but the aspirin keeps it at a low intensity and easily handled by reliever medication if necessary.)
Part 2 of this blog (after the diary below) details experience of using beclomethasone, montelukast, salamol and salmeterol xinafoate.
Conclusion
While aspirin can never be seen as a substitute for modern asthma medicines, it can help under moderate weather conditions (see diary below). Its use helps with reducing intake of relievers such as salbutamol sulphate. Beclomethasone dipropionate should be avoided if collapses occur.
Diary:
January 2016: I have resolved to suck on a dispersible aspirin before taking a shower and before going out into cold night air. (It helps to sip some water at the time, if necessary.) This is working well.
Any negative effects? If an asthma attack is already underway, the immediate impact of aspirin might seem to worsen it slightly, for a second or two. If I can also get away from the asthma trigger (cold air with humidity), I then usually feel a good recovery in under ten minutes. Without taking the aspirin, the asthmatic tightness abates much more slowly, having an impact on normal activity.
Stubborn asthma. Occasionally, I still get a form of asthma that is not helped by moving into a warm room. (In fact, I remember one incident where I got no relief until I exited a warm building and was back in fresh air.) The tightness can continue to worsen, sometimes quite slowly, and also does not seem to be affected by aspirin, although a combination of aspirin and a hot drink has been remedial sometimes. Using salmeterol then becomes sensible.
Tip: Anticipation is important: dose with aspirin slightly in advance of times when the asthma tends to occur. (I also reduce the risk of early-morning asthma by taking a pill when going to bed.) Respond quickly when tightness in the chest is noticed. (It's been observed that migraine is also stopped best by aspirin if caught early.) Persevere: I have successfully quelled asthma by taking a second 300mg aspirin tablet when the first one didn't seem to be helping. Prescribed reliever (e.g. salmeterol) will be needed occasionally, but less so as you become practiced at managing with aspirin. When using aspirin as a reliever in winter (e.g. out in public) it is advisable to also find a warm location, and have a hot drink for best results. (Honey and concentrated lemon in hot water is good in the night; tea or fresh filter coffee by day.)
PREVIOUS DIARY:
12/01/2015. New remedy since 08/01/15: Aspirin approximately 3 times daily has made me asthma-free continuously in cold, wet January weather and while having flu with a bad cough. This fact flies in the face of published information e.g. asthma.partners.org : Between 3 and 5% in an American study say that aspirin worsens their asthma. Even if this finding extrapolates well worldwide, there remains the possibility that between 95 and 97% can be helped by aspirin, if they are prepared to stop using prescribed preventer while they try it. (Please also see the two bullet-pointed comments at the very end of this blog.)
26/01/15. Aspirin seems to be most effective against wheezing at night (wheezing is recognized as a separate issue by some experts.) With wheezing gone almost completely now, my need for conventional asthma reliever has dropped to a minimum: I have used Serevent only 3 times since 08/01/15, when tightness in my chest occurred at night (triggered mainly by sudden exposure to cold, damp air in the bathroom.) My aspirin 'regimen' has been 2 or more aspirin in the evening (1 of them before bed); 1 to 2 pills in the morning, if required. (Adults can safely take up to 13 x 300mg aspirin daily.)
03/02/15. Having a late shower last night triggered a severe asthma which the aspirin did not remedy. I used Salamol reliever and had a nightmare later. If other asthma still occurs that is not handled by aspirin, I will use Serevent only in future. I will avoid steamy showers in a cold bathroom at night.
Interim diary is pasted near the bottom of this page
A final observation for 2015 (in a forum discussion.): I would add that the last flat I had was very close to the seafront and it seems that the quality of air on cold seafronts is such that it brings me asthma in cold weather. I noticed this year that my asthma was being triggered at a favourite beach spot as soon as clouds rolled in and the wind was unseasonably cold. I'd be almost fully asthmatic by the timed I'd climbed up the steep bluff to my car. Once in the car, I'd recover quite quickly if I could take an aspirin. On warm days at the same spot, I could muck around in the chilly water for hours on end, with no hint of asthma at any time.
05/06/2016. I have started using beclomethasone again, once per day to improve sleep. Aspirin was still working as described, but it was not preventing me from waking too early in the morning because of a slowly increasing asthma if the bed became cold. It was becoming too burdensome to have a hot honey drink with aspirin every time this happened. So far, one puff of beclomethasone, in the afternoon, has had good effect and I use the aspirin much less.
06/06/2016. The eerie sensation that precedes blacking out has returned after 3 days back on beclomethasone, but only briefly. The preventer is definitely the primary cause of the blackouts.
23 June 2016. I just had one of the blackouts that got this blog started a couple of years ago. I recognized it coming, turned off the stove-top and lay down quickly. It passed in a few minutes. Am now certain that beclomethasone gives me blackouts. Have been using less than one puff per day.
26 June 2016. I was waking from an afternoon nap when I went into a severe blacking out state (quite terrifying and feels life-threatening.) I managed to stay conscious by breathing faster and moving my body intuitively. I did not feel that I could get up for water until it passed. Am now 100% certain that Beclomethosone was the cause of the blackouts that began in 2011.Discretionary note: a Wikipedia summary says that people fall into different groups according to how they respond to aspirin.
 |
Montelukast side effects include rare but important: "Suicidal thoughts and actions." There are also web forum accounts of children becoming unmanageable while taking Montelukast (e.g. see mumsnet, kids-on-Montelukast and facebook/aspirin-for-asthma)
|
 |
| Aspirin stopped night-time severe wheezing abruptly, and it's never been a problem since. |
Part ii) Use of steroid asthma drug beclomethasone dipropionate (Qvar®) was associated with recurrent collapse.
The fine print tells us that asthma reliever salbutamol sulphate can cause collapse in children by inducing a drop in blood pressure. (Salbutamol is listed by the W.H.O. as an Essential Medicine and prescribed widely.) However, use of steroidal asthma preventer beclomethasone dipropionate coincided with recurring collapses. (Chewing gum and Polo mints have triggered a collapse/the warning-sensation of a potential collapse, but a reaction to chewing gum or Polo mints never occurred before beclomethasone was used.)
Blackouts, which I'd never had before, occurred after I began to use inhaler pumps for asthma in 2011. The fainting/collapse was not frequent, with only about 5 incidents in a year, but it was very disruptive and made me wonder if fatal situations might arise. I stopped using my brown 'preventer' puffer and the blackouts stopped.
Reluctantly, I started to use the brown puffer again in July 2014, when cold weather was worsening the asthma: The grim sensation that precedes a blackout then occurred after 7 days. Again, I stopped using beclomethasone, but then started to have severe wheezing and asthma in the night, waking in a struggle for breath. Wheezing at night was more severe than I'd ever experienced. (2 tbsp. of honey before bed was no longer helping in any way.) There were periods of extreme lethargy during recovery.
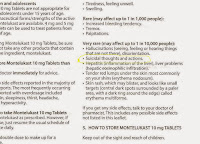 |
| Fig. 1. Rare but important: "Suicidal thoughts and actions." (Click to enlarge) |
When montelukast no longer seemed to be the remedy I'd been looking for, I stopped using any preventer and tried a more frequent use of salbutamol (reliever) instead. Again, I sensed no threat of blackouts but asthma at night soon worsened, and the relief given by salbutamol was only lasting for 2 or 3 hours.
 |
| Fig. 2. Salamol might cause collapse. (Click to enlarge) |
I feel fortunate that aspirin has enabled me to step down my use of prescription medicines, and to stop all use of steroid medication.
Other observations (with some repetition.)
As mentioned above, after three years of using beclomethasone sparingly, I still wanted to be certain that salbutamol sulphate had not actually been the cause of collapses. (Salbutamol had been my 'reliever' medication when black-outs had first occurred in 2011.) I read on the internet (ref. Wikipedia.org) that salbutamol is a known cause of collapse by causing a drop in blood pressure.In October 2014, when montelukast (a non-steroidal preventer) was suddenly giving a poor performance after a month of good result, I tried using salbutamol alone. (I didn't want to start taking beclomethasone again.) As I expected, no signs of blacking-out occurred, but the salbutamol was giving relief for only 2 or 3 hours in the wintry nights. I visited the NHS surgery and a new doctor prescribed a long-acting reliever called salmeterol to get me through the nights (marketed as Serevent).
For two days I seemed to do well on salmeterol, but then wheezing in the night became a problem again. Alarmed, I found on Google that salmeterol can cause an increase in wheezing because it is powdery and can accumulate in the lungs. (This problem doesn't occur now with well-spaced dosing, i.e. only one puff daily at the most, usually less.)
Relievers do only one helpful thing in one's lungs: They open the airways for a while by causing smooth muscle to relax. They do not do anything to stop the lung inflammation that is the root cause of asthma, and for which inhalation of a steroidal substance has been the primary treatment worldwide. I had discovered that I cannot manage asthma well with relievers alone ("not surprising", I hear you say), and began to wonder if there was any escape from using steroidal substance as preventer.
In December 2014, I put beclomethasone to the test one more time (the third time). I used it again faithfully and with no other medicines. (I also did not chew any gum, because there are anecdotes that gum can cause blackouts.) Within a week, I was getting the familiar, eerie sense of an impending blackout. Conclusion: steroidal preventer does not go well with my physiological make-up. Luckily, aspirin helps me a lot instead.
Diary of 12/12/2014: Being back on steroidal, I'm finding the predictors of blackouts returning - perhaps use of steroid for preventing asthma can exacerbate a tendency to have low blood pressure, with unpleasant consequences (see below.)
------------------------------------------------------------------------------------------------------------
What follows below is the 'old' blog. Its message has been confirmed three times: The sensation that precedes blacking out has come back each time I resumed use of beclomethasone, and complete blackouts occurred when I persisted in using it.
May 2016: It should be mentioned that an ingredient in chewing gum and in Polo mints also can trigger the blackouts described. I used to eat a lot of Polo mints in the three years before I first used beclomethasone. However, the problem only developed when using beclomethasone.
p.s. February/March 2018: There seems to be an ingredient in Jakeman's Throat and Chest Lozenges that can trigger the blacking out.
What follows below is the 'old' blog. Its message has been confirmed three times: The sensation that precedes blacking out has come back each time I resumed use of beclomethasone, and complete blackouts occurred when I persisted in using it.
May 2016: It should be mentioned that an ingredient in chewing gum and in Polo mints also can trigger the blackouts described. I used to eat a lot of Polo mints in the three years before I first used beclomethasone. However, the problem only developed when using beclomethasone.
p.s. February/March 2018: There seems to be an ingredient in Jakeman's Throat and Chest Lozenges that can trigger the blacking out.
The original blog follows below Inhalation of a steroid is generally regarded as almost risk-free, while doses taken orally or by injection might have an impact. However, there are research findings that do not put inhaled steroids into a 'harmless' category (see bit.ly/ICSdanger and bit.ly/pneuflut.)
Asthma-preventer beclomethasone dipropionate has been associated with collapse.
My blood pressure was found to be low when I
offered a blood donation in the early 1980's, and I was turned away. However,
low b.p. was never problematic for me until I started using Beclomethasone Dipropionate for asthma. I was housed in a cold building in 2011 and a GP's nurse
issued me with preventer and reliever pumps. For a year and five months I used
the preventer pump (with beclomethasone) much more than the reliever, as
recommended.
Beclomethasone is a synthetic hormone known as a glucocorticoid (GC), a type of 'corticosteroid'. One natural function of a GC is to suppress inflammatory responses and that is why a synthetic GC can be used to counter asthma: by suppressing inflammation in the lungs. A natural GC produced in one's body (in the adrenal cortex) influences more than one important physiological process. It follows that more than one effect might take place after inhaling a synthetic GC.
Some time after starting to use beclomethasone, I had a fainting experience. It began with a dreamlike state, as if slipping back into a nightmare. A loss of consciousness followed within a minute. The fainting happened again a few weeks later and I would say that the word 'deathly' best describes the intoxicated feeling that occurs just before fainting. One feels uncertain where things are headed. I mentioned the problem to my GP and also told him that I had eaten some cold meat just before it happened. I had read that ingested nitrates (found in most cold meats) can cause fainting by lowering blood pressure. He started to suggest a series of food tests but I decided to see how things developed.
More fainting occurred at unpredictable times, often months apart. In December 2012, an episode occurred as I arrived back to a work-station after a short tea break. Someone saw me lie down on the floor and advised me to raise my legs. That did prevent me from going completely unconscious, by raising the blood pressure in my upper body. In January 2013, I passed out again at home after drinking some coffee and then getting up quickly. As I woke up, I had a sense for the first time that the asthma medication was at the root of the problem (not unlike the way that you know when alcohol has given you a pleasant form of intoxication.) I was feeling lethargic that morning after using reliever the night before (to go out on a bicycle in cold damp air.) The Salamol reliever I used has no steroid content, but I had also recently used beclomethasone. As usual, the blackouts had only happened twice in a couple of months, but that seemed to fit in with having always used the beclomethasone pump sparingly.
More than one factor can trigger a quick drop in blood pressure, leading to fainting (including, believe it or not, chewing gum) but I believe now that the beclomethasone was giving me a bodily condition in which normal fluctuations in blood pressure were becoming exaggerated. The tea, nitrates, coffee etc. might have been precipitating factors, but the beclomethasone was causing the vulnerability.
Information on the internet helped me piece together a possible explanation. A search for 'inhaled Corticosteroids- Systemic Side Effects' found the following (on asthma.about.com):
Beclomethasone is a synthetic hormone known as a glucocorticoid (GC), a type of 'corticosteroid'. One natural function of a GC is to suppress inflammatory responses and that is why a synthetic GC can be used to counter asthma: by suppressing inflammation in the lungs. A natural GC produced in one's body (in the adrenal cortex) influences more than one important physiological process. It follows that more than one effect might take place after inhaling a synthetic GC.
Some time after starting to use beclomethasone, I had a fainting experience. It began with a dreamlike state, as if slipping back into a nightmare. A loss of consciousness followed within a minute. The fainting happened again a few weeks later and I would say that the word 'deathly' best describes the intoxicated feeling that occurs just before fainting. One feels uncertain where things are headed. I mentioned the problem to my GP and also told him that I had eaten some cold meat just before it happened. I had read that ingested nitrates (found in most cold meats) can cause fainting by lowering blood pressure. He started to suggest a series of food tests but I decided to see how things developed.
More fainting occurred at unpredictable times, often months apart. In December 2012, an episode occurred as I arrived back to a work-station after a short tea break. Someone saw me lie down on the floor and advised me to raise my legs. That did prevent me from going completely unconscious, by raising the blood pressure in my upper body. In January 2013, I passed out again at home after drinking some coffee and then getting up quickly. As I woke up, I had a sense for the first time that the asthma medication was at the root of the problem (not unlike the way that you know when alcohol has given you a pleasant form of intoxication.) I was feeling lethargic that morning after using reliever the night before (to go out on a bicycle in cold damp air.) The Salamol reliever I used has no steroid content, but I had also recently used beclomethasone. As usual, the blackouts had only happened twice in a couple of months, but that seemed to fit in with having always used the beclomethasone pump sparingly.
More than one factor can trigger a quick drop in blood pressure, leading to fainting (including, believe it or not, chewing gum) but I believe now that the beclomethasone was giving me a bodily condition in which normal fluctuations in blood pressure were becoming exaggerated. The tea, nitrates, coffee etc. might have been precipitating factors, but the beclomethasone was causing the vulnerability.
Information on the internet helped me piece together a possible explanation. A search for 'inhaled Corticosteroids- Systemic Side Effects' found the following (on asthma.about.com):
"While uncommon, a number of systemic effects can occur with inhaled
corticosteroids. Generally, there is a higher risk with increasing doses of
inhaled corticosteroids. Potential asthma medication side-effects with inhaled
steroids include:
- Poor Growth
- Decreased Bone Density:
- Disseminated Varicella Infection (chickenpox that spreads to organs)
- Easy Bruising
- Cataracts and Glaucoma
- Adrenal Gland Suppression (AGS)"
Low blood pressure is not mentioned in the list above but the following list was found through the web link: Adrenal Gland Suppression (AGS): (- link now disabled)
- Decreased ability to respond to emotional or physical stress
- Fatigue
- Joint pains (arthralgias)
- Low blood pressure (hypotension), which may cause light-headedness or fainting when you stand after sitting or lying down
- Muscle pains (myalgias)
- Nausea and vomiting
- Shock
- Weakness"
The list of symptoms of Adrenal gland suppression (AGS) made sense to me
in more than one way. I'd recently started to notice fatigue, unusual leg
muscle pain and sore joints, as well as having the fainting episodes. I had blamed the sore joints
on cycling but it had seemed a different sensation, and worse, than I was used
to.
Recently I found a web page which pulls no punches about the
negative aspects of steroidal medication. It does not distinguish between side
effects from injection of steroids and those that come with inhalation of
smaller doses, but the warnings should surely be considered: http://www.healthline.com/health/glucocorticoids#SideEffects.
How would exogenous adrenal gland suppression cause low blood pressure and fainting? (exogenous = caused by an agent from outside the body)
Steroidal medication lowers the natural production of
cortisol in the adrenal glands by interacting with natural feedback systems. Cortisol is one's own (endogenous) steroid, made by cells in the zona fasciculata. Medical introduction of
synthetic steroid into the blood causes a down-regulation of cortisol
production in the zonae fasciculatae. The resulting 'suppression of the adrenal
glands' (not forgetting that we are only talking about the zonae fasciculatae)
always happens because less cortisol is needed by the body when a substitute is
present (from outside the body.) As with other hormones, total blood concentration of any glucocorticoid is
maintained within precise limits by natural feedback mechanisms.
Asthma.about.com says that the side effects of adrenal gland suppression will only be noticed when the supply of the synthetic GC has stopped. That is because the adrenal glands need time to recover normal production of natural GC (i.e. cortisol) when the exogenous supply of synthetic has stopped. During the 'recovery time', there is insufficient total glucocorticoid in the blood, i.e. [endogenous cortisol] + [synthetic GC]. This is when symptoms in the AGS list might occur.
If a patient maintains a regular intake of steroid as medication, there will be no suffering of AGS unless the exogenous supply is stopped abruptly, leaving the body reliant on suppressed adrenal glands which will need time to recover. It seems possible that an asthma patient who generally prefers to minimize the intake of steroids might feel the AGS symptoms whenever he/she stops using the pump, or skips doses.
Information on Wikipedia makes it obvious why a temporary shortfall in total blood GC can lead to problems with blood pressure:
Asthma.about.com says that the side effects of adrenal gland suppression will only be noticed when the supply of the synthetic GC has stopped. That is because the adrenal glands need time to recover normal production of natural GC (i.e. cortisol) when the exogenous supply of synthetic has stopped. During the 'recovery time', there is insufficient total glucocorticoid in the blood, i.e. [endogenous cortisol] + [synthetic GC]. This is when symptoms in the AGS list might occur.
If a patient maintains a regular intake of steroid as medication, there will be no suffering of AGS unless the exogenous supply is stopped abruptly, leaving the body reliant on suppressed adrenal glands which will need time to recover. It seems possible that an asthma patient who generally prefers to minimize the intake of steroids might feel the AGS symptoms whenever he/she stops using the pump, or skips doses.
Information on Wikipedia makes it obvious why a temporary shortfall in total blood GC can lead to problems with blood pressure:
"Cortisol, ... a glucocorticoid ... is released
in response to stress and a low level of blood glucocorticoids. Its primary
functions are to increase blood sugar through gluconeogenesis; suppress
the immune system; and aid in fat, protein and carbohydrate metabolism.[2]
It also decreases bone formation, and ... increases blood pressure by increasing the sensitivity of
the vasculature to epinephrine and norepinephrine. ... In the absence of cortisol,
widespread vasodilation occurs. (ref. https://en.wikipedia.org/wiki/Cortisol)" It seems obvious that any interruption in blood concentration of cortisol might cause fainting because of a drop in blood pressure resulting from "widespread vasoldilation" (widening of the blood vessels.)
A friend of mine
had protested that my blackouts were probably due to low blood sugar, while I
was focused on low blood pressure. It turns out that under-production of
cortisol leads to both conditions.
Conclusion
There is nowadays some acceptance that inhaled steroids can have dangerous side-effects. Apply a hormone to a body surface and less of that hormone type will be produced naturally in the body. This is understood as 'down-regulation". The steroid Budesonide now comes with a flyer that declares rare side-effects as follows: "too much or too little cortisol in the blood" and "underactive adrenal gland".
The effects of adrenal gland suppression can become evident after a patient begins to use steroids for relief from inflammation. Incidents of low blood pressure can develop when steroid dosage is then interrupted. Frequent, regular dosing is advised because the symptoms of adrenal gland suppression are expressed only when exogenous dosage is stopped. (Total blood GC drops when exogenous dosage is stopped because the adrenal glands need time to 'wake up' again.) My own side effects from using beclomethasone did match the description of 'exogenous adrenal gland suppression', and the symptoms surfaced repeatedly, possibly because I did not maintain regularity in using the steroid.
It will be difficult to detect when an individual is likely to suffer important side effects from using a synthetic GC because some of the side effects develop gradually. For example, poor growth and decreased bone density would not be noticed for months or even years. A test for low blood pressure at the doctor's surgery would not be a reliable way to identify those patients who might be affected in the way described, because a recent BBC news report stated that some people have elevated b.p. whenever they visit a doctor, caused by anxiety about the visit.
Conclusion
| Budesonide is another synthetic GC and this 2018 flyer mentions side effects that would cause low blood pressure. |
The effects of adrenal gland suppression can become evident after a patient begins to use steroids for relief from inflammation. Incidents of low blood pressure can develop when steroid dosage is then interrupted. Frequent, regular dosing is advised because the symptoms of adrenal gland suppression are expressed only when exogenous dosage is stopped. (Total blood GC drops when exogenous dosage is stopped because the adrenal glands need time to 'wake up' again.) My own side effects from using beclomethasone did match the description of 'exogenous adrenal gland suppression', and the symptoms surfaced repeatedly, possibly because I did not maintain regularity in using the steroid.
It will be difficult to detect when an individual is likely to suffer important side effects from using a synthetic GC because some of the side effects develop gradually. For example, poor growth and decreased bone density would not be noticed for months or even years. A test for low blood pressure at the doctor's surgery would not be a reliable way to identify those patients who might be affected in the way described, because a recent BBC news report stated that some people have elevated b.p. whenever they visit a doctor, caused by anxiety about the visit.
____________________________________________________________________________
Scrap-book
- In that asthma.partners.org article they say that between 3 and 5% of asthmatic people say that aspirin worsens their asthma. Just one actual study is mentioned, done at Brigham and Women's Hospital (which showed increase of leukotrienes in people who claimed to be aspirin-sensitve asthmatics.) Working from these small percentages, the article nevertheless develops a general discouragement of the use of aspirin, as do other web pages. More empirical work needed here? After all, one person claimed that looking at facebook triggers his asthma (see The Lancet, Volume 376, No. 9754, p1740, 20 November 2010 'Facebook: a new trigger for asthma?') and the story gained wide publicity, but do asthmatics generally avoid using facebook as a result? How about a study to see if asthmatics can find a positive response to aspirin (after pausing their usage of conventional drugs, of course?)
"I know what people mean about aspirin 'making their asthma worse': if you take aspirin in the middle of a bad attack you sometimes can sense the way it alters your physiology and that can bring a panic because it's a stressful moment anyway. However, the effect subsides quite quickly and then the aspirin works favourably. I'm sure something similar takes place when second-hand smoke affects an asthmatic: it's mostly a panic reaction that is triggered, which be handled if one calms oneself and sits still for a bit (everyone gets that tight-chested spasm when smoke hits the airways without warning, but it seems much worse if you're already in a tight-chested state because of asthma.) I smoked for 20 years and was completely asthma free, having had asthma once before those 20 years, and long since I stopped smoking in ca. 1996. Cold, humid air causes my asthma; smoking didn't at all."
- One last point, they (asthma.partners.org) say that NSAIDs do not have any effect on inflammation in the lungs. They do not quote the source of this information. It would be very difficult to prove that some inflammation in somebody's lungs was no better after taking aspirin. Hi-tech observational techniques would be needed to even start to answer that one.
END Note (by a friend): "With me if I take a brufen I get an almost immediate asthma attack which can take a few hours to subside and go away. Well not for some time now because I just daren't take brufen at all in case I have an asthma attack; so whether or not it still affects me the same way I just don't know, but I daren't experiment and try it out to see if it does, because I remember how it used to affect me."_____________________________________________________________________
"it sounds like the brufen is affecting the same system in the body that's involved with asthma, as is the aspirin.""About a panic reaction - yes. but I know with brufen it is just not a panic reaction, it is a physical reaction. I remember feeling panicky because of the asthmatic reaction and not being able to breathe and the hot almost burning sensation in my lungs, I remember feeling panicky but having to calm myself and just bear the symptoms until they eased and went away."
This article makes interesting general points, not only about people in polluted areas: cnn.com/pollution.asthma.suicide/
Diary (contd.):
06/02/15. I went out on my bicycle in the near-freezing windy weather and had minimal asthma at the end of a route which previously would challenge me seriously. My energy level on the bicycle is much higher than before. Conclusion: aspirin seems to be effective in improving the overall condition of the lungs, eliminating wheezing and reducing the incidence and severity of asthma strikingly.
22/02/15. Since I started dosing with aspirin, I have used prescription asthma reliever only 7 times in 45 days and have used no preventer at all. Before 08/01/15, I was inhaling beclomethasone twice daily and still needing reliever occasionally.Tip: Dose with aspirin slightly in advance of times in the day when the asthma tends to occur. Respond quickly when tightness in the chest is noticed. (It's been observed that migraine is also stopped best by aspirin if caught early.) Persevere: I have successfully quelled asthma by taking a second 300mg aspirin tablet when the first one didn't seem to be helping. Occasionally, prescribed reliever (e.g. Serevent) will be needed, but less so as you become practiced at managing with aspirin. When using aspirin as a reliever in winter (e.g. out in public) it is advisable to also find a warm location, and have a hot drink for best results. (Honey and concentrated lemon in hot water is good in the night, tea or fresh filter coffee by day.)
25/02/15. Today, morning temperatures have finally settled above the zero mark with a warm front moving in, and winter seems to be giving way to spring. Aspirin is proving very effective at these temperatures, driving back all asthmatic symptoms.
17/03/15 - SUMMARY. I've been through a run of asthma 'medicines' over 4 years and found that, with the exception of steroidal Beclomethasone, they were suddenly less able to give me stability last autumn (July), when the asthma began to worsen a lot. Moderate use of aspirin has greatly reduced the frequency and severity of my asthma attacks, in a reliable way. I now use no preventer at all, so my problem with a side effect of Beclomethasone is over. Sometimes, asthma with mild wheezing still sets in at night and then I have found relief with salmeterol: it's been a very low usage, only 13 puffs since 08/01/15; that's 13 puffs in almost 10 weeks. With practice, I might reduce that even further. (Serevent comes in a dry formula inhaler, with no propellant in the mix, and is a long-acting reliever. It doesn't relieve as quickly as salbutamol, but is good enough for most purposes.)
24/04/15 - Warm weather now has reduced the need for aspirin to one or two tablets daily. It seems that I will get through the summer with no need for salmeterol.
10/05/15 - I have not used salmeterol for a week, having a daily routine that is very much more active since 20/04/15. One observation worth mentioning is that I can sense when cold, moist air is being driven inland from the sea by winds: There is a pre-asthmatic sensation in the lungs that confirms the weather reports on TV. The same sensation occurs when entering a large refrigerator at work, but it hasn't developed into an asthma attack, because I don't stay in there for too long. // I still take an aspirin in the mornings, and the physical activity later at work also seems to build my resistance to asthma. Conclusion: aspirin and sustained physical activity work well together to build up 'resistance' to asthma. Home-brewed filter coffee in the morning is beneficial in the cold months, although I feel less dependent on it now. (Green or rooibos tea, or honey and lemon in hot water, works at night if sleep is broken.)
16/06/2015. Last week I had one of the black-outs, after being off beclomethasone for 6 months. I had recently stepped up my use of salmeterol, using it once before bed on each of 3 days consecutively. (A lot of cool humidity had been occurring here on the South West coast, causing a slow build up of asthma in the evenings.) However, I had also been chewing gum a lot for a few weeks before this black-out. Chewing gum has been reported on the internet as a cause of blackouts. Either gum or salmeterol are posing the same risk that beclomethasone had, although with a much lower frequency. (When I last tried using beclomethasone again, last year, I got a premonition of blacking out after only a day. It's a feeling that comes and goes during the day, but cannot be 'fought off' when a real blackout begins.) I have felt more sound physically during the last six months, and had no other black-outs. Having stopped the chewing gum habit now, the risk seems to be gone altogether.
29/07/15 - I've had no sensations associated with blacking out since I stopped using chewing gum. Chewing gum does seem to have played a role, but I hesitate to let beclomethasone off the hook as a more potent cause.
26/08/15 - Comparing the situation now with the poor asthma management I had in July 2014, regular use of aspirin has changed my physiology such that I can lead a normal life with reliance on a very low usage of salmeterol. Aspirin put a blanket on my symptoms very effectively. Not a quick cure but has given me the edge and I use just one medication now, at a greatly reduced frequency. Simply following a routine of prescribed steroidal preventer lnhalation can lead to a masking of the condition: I have become much more aware of how cold-sea humidity triggers my asthma. In these summer months I've used a maximum of 2 dispersible aspirin on some of the cooler days near the beach.
08/10/2015 - Since getting a compact dehumidifier, aspirin is working even better. They have recently appeared in ebay as '500ml portable dehumidifier'. They sell for about £20 and use minimal electricity, having no noisy compressor.
17/10/2015: I took a silly risk and wore a jersey that had become musty smelling from damp in a low drawer. It triggered tight asthma which did ease off with two aspirins, but my lungs were still uncomfortable at 3 am, so I used salmeterol. Apart from that, I had used no salmeterol for a week.Forum entry on 17/01/16: My suspicion of steroidal medicines made me cautious with prescription medications, but I had a very serious side-effect, nevertheless. Then a piece of luck: aspirin before bed stopped wheezing when it had become extreme at night in July 2014. Now, aspirin fends off asthma: I also take one before showering and one before going out for an evening in cold air. Every few days, an episode of stubborn tight chest has still been getting a grip, and then one puff of salmeterol sets me back to 'normal' for two days or more; back to coping by intake of aspirin.
My experience is: Some GP's will end every consultation with a reiteration of the standard procedure. I found that salmeterol actually CAUSED wheezing if I use it twice per day. In desperation, I googled the problem and, sure enough, salmeterol is known to do this because it is breathed in as a powder, and the build up of powder is the cause of the wheezing. My GP accepted this explanation during my last visit, but he ended the visitation by reading aloud that I must use salmeterol "TWICE DAILY" after collecting my repeat prescription. I cope very well now with single puffs of salmeterol, because I fend off most asthma quite well with aspirin, only 'resorting' to salmeterol once every few days (when stubborn tight chest occurs, depending on the weather.)
More info:




